Medical Billing
We fix the patient appointment for the Medical professional based on the availability of the providers & requirement of the patients at the time and date requested by patients.
Insurance Eligibility & Verification:In the absence of proper eligibility and benefit verification countless downstream problems are created; delayed payments, rework, decreased patient satisfaction, increased errors, and nonpayment. To avoid these problems, MAE Health Care provides a remotely hosted Centralized Eligibility Unit for Hospitals and Faculty Practice Plans. The solution consists of MAE Health Care deploying staff, technology, management and expertise with the objective of delivering high quality cost effective patient insurance eligibility and related services.
Synergetics Pro's Eligibility Verification Services has the potential to:- Reduce A/R days
- Increase cash collections by reducing write-offs and denials
- Receive Schedules from the Hospital via EDI, email or fax
- Verify coverage on all Primary and Secondary (if applicable) Payers by utilizing sites like WebMD, Payer Web Sites, Automated Voice Responses and phone calls to Payers
- Contact patient for information if necessary
- Provide the client with the results which include eligibility and benefits information such as member ID, group ID, coverage end and start dates, co-pay information and much more
- Obtain Pre- Authorization Number
- Obtain referral from PCP
- Enter/update Patient demographics
- Remind patient of POS collection requirements
- Inform client if there is an issue with coverage or Authorization
- Medicaid Enrollment
Revenue Cycle Management
MAE Health Care provides a Comprehensive Revenue Cycle Management (RCM) services to Providers and Hospitals. We accelerate people, processes and technology to provide operational and financial solutions to our clients. Our goal is to help you maximize reimbursement and reduce expenses. Our services include, Patient Registration, Medical Coding, Charge Entry, Payment Posting, Denial Management and Accounts Receivable (AR) Follow-Up
Demo, Charge Entry & Payments posting – MAE Health Care is skilled in all aspects of medical billing and our experience includes Medicare, Medicaid, HMO, POS, EPO, PPO, Worker's Compensation and private indemnities. Our services include:
- Patient Registration
- Charge Entry
- Payment Posting
- Denial Capturing
- Patient Statement (Reconciliation)
- Refunds
- Provider Data Updates
MAE Health Care have experience in working on all leading practice management systems includes: Medic, ADS (Advance Data System), Centricity, E-Clinics, IMS-Meditab, Medisoft. Also we can adopt rapidly to any web based or other software that you provide.
Pre-AuthorizationDepending whether patient's policy is an HMO or a PPO can affect whether or not certain procedures or treatments are covered without prior authorization. So, if we are unsure what services are and are not covered by patients health insurance plan, So we make sure by contacting the patient's insurance and verifying the policy benefits to avoid being patient's left with extra medical expenses
Provider (We) requests pre-authorization, so patient or Providers office need do nothing other than visit the patient and ask them if they have pre-authorization if necessary for that service. We would present evidence of the necessity of the procedure by supplying the insurer with a report, lab and/or test results, scans, x-rays, photographs or other supporting materials requested & collected from provider that indicate that the procedure is necessary.
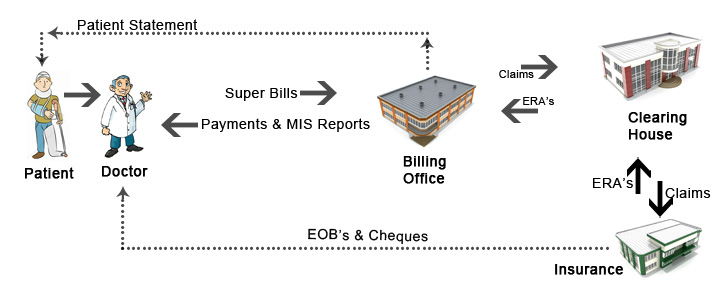
Claims SubmissionMAE Health Care always insist their claim for submitting electronic claims which would fetch reimbursement at the least time from 72 hours compared to a paper billing that may take up to 3 weeks. Electronic submission reduces errors and lost of claims by 98%. Transmission is fully encrypted and compliant with HIPAA rules and guidelines.
Quality AssuranceMAE Health Care follows a series of steps to ensure high standards of quality in all our healthcare services. To minimize error rates and reduce the risk of denials, Our expertise team reviews all claims before submission. The most common reasons for claims rejections are specified in a log list compiled by our billing staff. With the help of this reference records, we track trends on remittance advice. We monitor and evaluate these records in order to resolve the problems that are causing the denials and rejections for your practice. This way, you get increased revenue through reimbursements and reduce the risk of future claims rejections.
Every month, we hold billing review meetings where the entire team involved in billing processes is present. Every person involved in data entry, billing and payment posting, coding and documentation, denials review & AR participates in the monthly review which includes
- An analysis of trends from the claims review log
- An update of any recent changes in billing or coding practices, from recent newsletters of insurance carriers
- Current practice issues regarding the billing function.
Accounts Receivables
MAE Health Care objective is to improve your cash flow by reducing days in A/R and improving profitability, by increasing your collections ratio. We are skilled to identify patient accounts that require follow-up and take the necessary action to collect unpaid/underpaid claims.
Services Include:- Payer / Insurance Follow-up
- Self pay follow-up
- Receivables Analysis
- Denials Management
 Our Accounts Receivables Management services include:
Our Accounts Receivables Management services include:
- Professional Claims Billing
- Commercial & Federal Insurances Follow-Up
- Cash Posting
- Credit Balance Resolution
- Zero Balance Audit
- Receivables & Denials Management
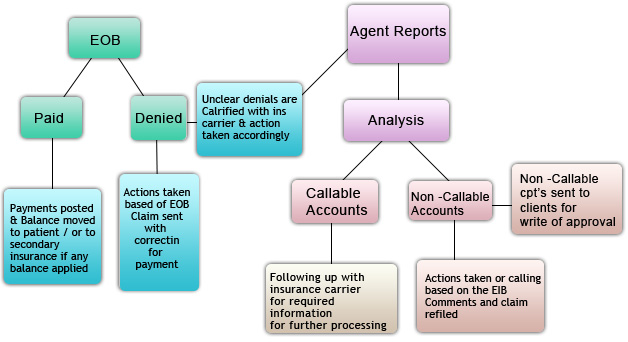
- Identification: Identify the claims on your AR Reports and understand your write off policy.
- Analysis: Experienced denial analysts will study your claims and identifying the various issues for non payment or under payment. This will include verifying the submission address, provider verification, etc.
- Collections: MAE Health Care will take necessary actions based on the Analysis Phase. This includes re-filing claims, initiating an appeal process where appropriate, etc.
MAE Health Care has its own module of tracking your denials where we will provide a comprehensive evaluation of processes, source of denials and reason. Maintaining tracking methods in-order to identify the type of denials based on carriers, times. This tracking systems always helps us to understand the trends followed by the insurance carriers for the respective denials, which in return generates your revenue at the same time will act as an detector to avoid the future denials.
Root - Cause Analysis of Claim DenialOur analysts helps uncover problems that lead to denials, both inside and outside the hospital / Clinics / Doctors, and provides robust tools to repair and resubmit denied claims and eliminate the root causes of denials within your revenue-cycle process.This will increase revenue, reduce denials and achieve efficiencies that were never before possible.
Denial Workflow DistributionOur analysts expedites the repair and resubmission of denied claims for cross-departmental teams. Our intelligent workflow engine applies client-specific logic to efficiently distribute denied claims requiring resubmission to the right departments and individual team members, while maintaining a detailed history of actions on all claims. Since many claims involve multiple teams, the intelligent workflow engine also supports communication and corrections across departments and facilities and continues tracking denied claims until they are resubmitted to the payor.
Following are the preventive measures of Denial from Occurring:- Review of managed care contracts that have a bearing on claims payment
- Prevention of physician reviews and thus denials
- Training programs to address specific denial issues
- Assessment of billing practices that may delay the claims process
- Providing a methodology to focus on denials and appeals
- Providing training for the utilization review and case management staff
- Self Pay Follow Up
- Provider Enrollment Issues
- Credit Balance Resolution
- Under Payment Analysis
So if you or your organization is suffering from staffing issues, unanticipated turnover or complex claims, MAE Health Care revenue recovery services are right for you.
 Contact Us : 408-385-2576
Contact Us : 408-385-2576


